INTRODUCTION-
Cervix is the lower most part of the uterus which is about 2.5 cm-3.5 in length. Half of it projects in vagina. It is subject to changes in the vagina, its pathogens and external environment..
Cancer of breast and cervix are the most common cancers among females. Cervical cancer accounted for 6-29% of all cancers among women in India. The estimated number of cervical cancer cases in the country in 2023 was more than 3.4 lakh, Patients of cervical cancer present with symptoms of irregular or continuous bleeding, post coital bleeding, offensive vaginal discharge, pelvic pain etc. It is associated with high morbidity and mortality.
The country records one new case of cervical cancer every four months, and one death every seven minutes.
Currently, roughly two thirds of the Indian women diagnosed with cervical cancer will die of the disease. This can only mean women are presenting with late-stage cancers.
PREVENTION OF CERVICAL CANCER
HPV and cervical cancer –
Human Papilloma Virus Infection (HPV) and its persistence are necessary and thought to be causative of cervical cancer. HPV is the most common viral infection of the reproductive tract. It is generally acquired by young women after the onset of sexual activity. The majority of HPV infections do not cause symptoms or disease and resolve spontaneously within 2 years. Persistent infection with high-risk HPV genotypes may result in cervical pre-cancer which, if untreated, may progress to cervical cancer. There are more than 150 types of HPV. Amongst these, 12 high-risk HPV types that are associated with cancers in humans are types -16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59). Worldwide, the most frequent HPV types are 16 and 18, with HPV 16 being the most common subtype.
It takes 10 years or longer from the time HPV infection is acquired to its progress to invasive carcinoma.
An HPV infection caused by oncogenic HPV types can linger for a long time and eventually transform healthy cells into cancerous cells if the body’s immune system eradicates it. A long-lasting HPV infection that increases the risk of cervical cancer occurs in 10% to 15% of women with cervix-based HPV infections. If not discovered and removed promptly, they might eventually become cancer.
Other Risk Factors for Cervical Cancer –
Several factors increase the risk of cervical cancer. Early age at onset of sexual activity, multiple sexual partners, tobacco smoking is identified as a risk factor for cervical cancer. High parity, smoking, nutrition and use of combined hormonal oral contraceptives for more than 5 years have been reported as major environmental risk factors for cervical cancer. Infection with other sexually transmitted diseases such as HIV, herpes, chlamydia, gonorrhea and syphilis increases the cervical cancer risk. The risk may also be increased in women taking immunosuppressive medications, women on a diet low in fruits and vegetables, women with long-term use of oral contraceptives and women in poverty.
Taking care of these factors may minimize risk of cervical cancer development.
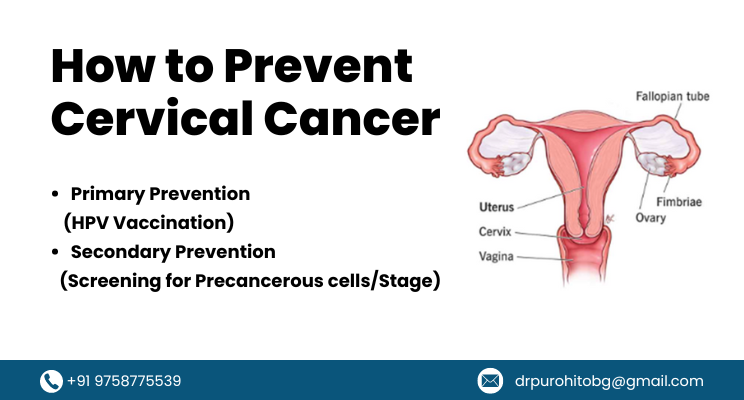
PREVENTION OF CERVICAL CANCER
Primary Prevention- Aims at elimination of root cause of disease process by neutralizing adverse effect of HPV on cervical cells.
Secondary Prevention– Aims at detection of disease in precancerous stage and treatment.
Primary Prevention (HPV Vaccination)-
Two prophylactic vaccines, a Quadrivalent vaccine which protects against HPV 6, 11, 16 and 18 and a bivalent vaccine which protects against HPV 16 and 18, are currently available and marketed worldwide for the prevention of HPV-related diseases. The quadrivalent vaccine Gardasil (Merck, USA) was licensed in 2006 and the Bivalent vaccine Cervarix (Glaxo Smith Klein, Belgium) was licensed in 2007.
Doses-HPV vaccines are most efficacious if administered before the onset of sexual activity, i.e. before first exposure to HPV infection.
Both vaccines are to be administered as a 0.5-ml intramuscular injection in the deltoid region from the age of 9 years onwards.
Two-dose vaccination (0 and 6 months) in girls aged 9–14 years appeared comparable to the standard 3-dose schedule in women aged 15– 25 years . The quadrivalent HPV vaccine can be administered according to a 2-dose schedule (0.5 ml at 0 and 6 months) for girls and boys aged 9–13 years. The third dose is essential if the second vaccine dose is administered earlier than 6 months after the first dose.
Alternatively, the vaccine can be administered according to a 3-dose schedule for those younger than 14 years (0.5 ml at 0, 2 and 6 months) and needs to be necessarily administered as a 3-dose schedule for those older than 14 years of age, wherein the minimum interval between dose 1 and 2 should be 1 month and the minimum interval between dose 2 and 3 should be 3 months.
The bivalent HPV vaccine is recommended as a 2-dose schedule (0.5 ml at 0 and 6 months) for girls aged 9–14 years and as a 3-dose schedule for girls older than 15 years (0.5 ml at 0, 1 and 6 months). If at any age the second vaccine dose is administered before the fifth month after the first dose, the third dose needs to be administered.
HPV vaccination was introduced into immunization programmes in Punjab and Sikkim (states) in 2016 by the respective governments.At the national level, it is being planned to be rolled out.
Aiming for Viksit Bharat by 2047 and with a sharp focus and providing momentum to Nari Shakti, Union Minister for Finance & Corporate Affairs, Smt. Nirmala Sitharaman proposed vaccination to prevent Cervical Cancer and amalgamation of various schemes for maternal and child care, when she presented the Interim Budget 2024-25 in Parliament.
The vaccination programme will be for girls in the age group of 9 to 14 years for prevention of cervical cancer. The Government will encourage this vaccination among the eligible categories, she added.
Secondary Prevention (Screening for Precancerous cells/Stage)–
Usually there is long gap between initiation of abnormal pathological process of proliferation of cervical cell and clinical manifestation of disease. By the time patient present with symptoms of cervical cancer disease has already advanced compromising prognosis.
Precancerous cervical cell changes usually have no symptoms. The only way to know if there are abnormal cells in the cervix that may develop into cancer is to have a cervical screening test. If symptoms occur, they usually include: vaginal bleeding between periods, after menopause, or during or after sexual intercourse.
What is cervical cancer screening?
The goal of screening for cervical cancer is to find precancerous cervical cell changes, when treatment can prevent cervical cancer from developing. Sometimes, cancer is found during cervical screening. Cervical cancer found at an early stage is usually easier to treat. By the time symptoms appear, cervical cancer may have begun to spread, making treatment more difficult.
There are three main ways to screen for cervical cancer:
- The Human Papilloma virus (HPV) test checks cells for infection with high-risk HPV types that can cause cervical cancer.
- The Pap test (also called a Pap smear or cervical cytology) collects cervical cells so they can be checked for changes caused by HPV that may—if left untreated—turn into cervical cancer. It can find precancerous cells and cervical cancer cells. A Pap test also sometimes finds conditions that are not cancer, such as infection or inflammation.
- The HPV/Pap co-test uses an HPV test and Pap test together to check for both high-risk HPV and cervical cell changes.
- Other modalities like Colposcopy may also be utilized.
When to get screened for cervical cancer
Cervical screening recommendations are developed by several organizations, including the United States Preventive Services Task Force (USPSTF) and the American Cancer Society (ACS). How often one should be screened for cervical cancer and which tests should be done will depend on age and health history. Because HPV vaccination does not prevent infection with all high-risk HPV types, vaccinated people who have a cervix should follow cervical cancer screening recommendations.
Age 21-29 years
USPSTF recommends getting your first Pap test at age 21, followed by Pap testing every 3 years. Even if sexually active, one does not need a Pap test before age 21.
Age 30-65 years
USPSTF recommends getting screened for cervical cancer using one of the following methods:
- HPV test every 5 years
- HPV/Pap co-test every 5 years
- Pap test every 3 years
Updated cervical cancer screening guidelines from ACS recommend starting screening at age 25 with an HPV test and having HPV testing every 5 years through age 65. However, testing with an HPV/Pap co-test every 5 years or with a Pap test every 3 years is still acceptable.
Older than 65 years
If women have been screened regularly and had normal test results, there is no longer need for screening. However, if recent test results were abnormal or have not been screened regularly, lady may need to continue screening beyond age 65.
Ready to take charge of your health? Contact us today at Dr. Purohit Clinic, the leading Obstetrics and Gynecology Specialist in Haldwani. Whether you need routine check-ups, preventive care, or specialized treatment, our team is here to provide compassionate and personalized care tailored to your needs. Visit our website at drpurohitclinic.com to learn more about our services and schedule your appointment.
Frequently Asked Questions
When to See A Doctor for Cervical Cancer?
1…All young girls between 9-14yrs for vaccination. If delayed up to 26 yrs.
2…For cervical cancer screening at age 21 and every three to 5 year thereafter till 65 yrs. This is applicable to all women irrespective of vaccination status.
3. Usually, there are no symptoms or signs of early-stage cervical cancer. Thus, it is required to book an appointment if any of any advanced cervical cancer symptoms and signs are seen, such as-
Bleeding from the cervix following sex, in between periods, or following menopause.
Bloody, watery, and foul-smelling vaginal discharge.
Pain during sexual activity or in the pelvis.
What is Pep test?
It is very simple test used as an OPD procedure. Cervical tissue scrapping are subjected to cytological test to detect pre-cancerous/ cancerous cells. It is painless test takes just 5-10 minutes.
HPV test– simple procedure in which cervical or vaginal tissue scrapping is used to detect HPV .It can be done along with pep test in same sitting.
How is cervical cancer diagnosed?
Cervical cancer is diagnosed through screening tests such as the HPV test, Pap test, and HPV/Pap co-test. If abnormal cells are detected, a follow-up procedure called colposcopy may be conducted to examine the cervix more closely and take a biopsy if needed.
Dr. R C Purohit
MBBS,DGO,MS